Why Does PMS Get Worse With Age?
Do pms symptoms get worse as you get older? For many women, the mood swings become more intense, the bloating more persistent, and the fatigue more debilitating in their 30s and 40s. Understanding why does pms get worse with age involves looking beyond simple hormones to consider lifestyle, stress, and the transition toward perimenopause.
1. Why PMS Worsens After 30
The shift isn't just about time; it's about accumulated physiological and external pressures that exacerbate the monthly hormonal fluctuations.
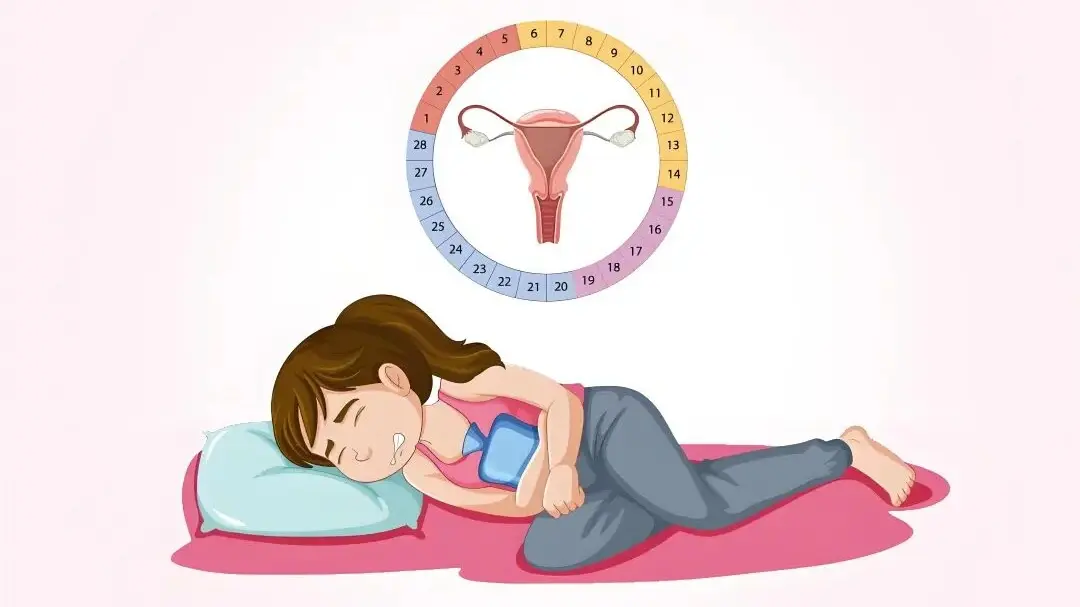
1.1 PMS Getting Worse with Age
The core of PMS lies in the dramatic shift between estrogen and progesterone in the luteal phase. As women approach their late 30s and 40s (the perimenopausal transition), ovarian function begins to decline. Instead of a smooth decline, hormone secretion becomes erratic. This instability especially in progesterone, which has a calming effect can lead to severe mood swings. If you notice your pms mood swings worse with age, this period of fluctuating hormones is often the primary culprit, causing intense anxiety, depression, or irritability.
1.2 Chronic Stress and Adrenal Fatigue
Mid-life often brings peak career demands, family responsibilities, and financial pressures. Long-term stress increases cortisol production. When the body constantly produces cortisol, it can "steal" precursors needed for sex hormone production (known as the "pregnenolone steal" pathway). This stress-induced hormonal imbalance interferes with the delicate estrogen/progesterone ratio, lowering the body’s tolerance for hormonal shifts and creating a vicious cycle where stress amplifies PMS symptoms.
1.3 Cumulative Lifestyle Impact
- Dietary Imbalance: High intake of salt and sugar exacerbates bloating and water retention. Excessive caffeine or alcohol can worsen anxiety and breast tenderness.
- Lack of Exercise: Reduced physical activity impairs blood circulation and toxin elimination, contributing to fatigue and pain.
- Poor Sleep: Chronic sleep deprivation lowers serotonin levels, directly contributing to severe moodiness and abnormal appetite during the premenstrual phase.
1.4 Overlap with Underlying Health Conditions
Sometimes, what feels like worsening PMS is the emergence or exacerbation of other conditions. These can mimic or compound PMS symptoms: Thyroid dysfunction (hypothyroidism) causes fatigue and weight gain; undiagnosed depression or anxiety disorders can make the emotional symptoms of PMS feel dramatically more pronounced; and conditions like Endometriosis or PCOS can lead to increasingly severe pelvic pain and hormone imbalance.
2. Can You Still Have PMS on Birth Control?
Many people take the pill hoping it will resolve menstrual discomfort entirely, only to find they still experience symptoms. This leads to the question: do you still experience pms on birth control?
The Reason Why Pms Symptoms Still Occur After Taking Birth Control Pills
Combination birth control pills (COC) work by suppressing natural ovulation and replacing your fluctuating natural hormones with a steady, low dose of synthetic hormones. While this typically alleviates the severe symptoms caused by natural hormone dips, some women still report pms while on the pill for a few reasons:
- Hormone-Free Week: During the placebo week, the sudden drop in synthetic hormones can cause withdrawal-like symptoms, which can feel identical to PMS.
- Sensitivity: Some individuals are highly sensitive to the specific synthetic progestin in their pill, which can trigger PMS-like mood swings (sometimes referred to as PME, or Premenstrual Exacerbation).
- Underlying Factors: The pill does not address stress, poor diet, or adrenal issues—the underlying causes that contribute to severe PMS as you age. Thus, can I still get pms on the pill? Yes, because the other exacerbating factors remain active.

3. What Tea is Good for PMS and Mood Swings?
Whether you are seeking relief from age-related worsening symptoms or asking what tea is good for pms to supplement medication, herbal remedies offer a holistic path toward balance. Traditional Chinese Medicine (TCM) attributes PMS to internal imbalances like Liver Qi Stagnation, Kidney Qi Deficiency, or Blood Stasis.
- Rose Bud Tea: Known for regulating Qi (energy) and blood. Its volatile oils, including citronellol and geraniol, provide natural aromatherapy, making it an excellent tea for pms mood swings by soothing anxiety and regulating the hypothalamic-pituitary-ovarian axis.
- Ginger Tea: Contains anti-inflammatory compounds. Often consumed with brown sugar in TCM, ginger helps warm the body and promote blood circulation, effectively relieving menstrual pain and combating the fatigue associated with PMS.
- Goji Berry (Wolfberry) Tea: Particularly Black Goji. These berries are potent antioxidants used to nourish the Liver and Kidney Qi, improving overall hormonal balance, reducing fluid retention, and addressing symptoms like poor sleep and menstrual irregularity.

Laicuherb's Blend: The Best Tea for PMS Mood Swings
For a full-spectrum solution, a scientifically formulated blend is often superior to single herbs. Laicuherb's PMS tea incorporates multiple botanicals in precise ratios, offering a powerful tea for pms relief that targets all facets of age-related worsening symptoms.
This blend combines warming, Qi-regulating, and blood-nourishing herbs—like Angelica, Red Dates, and Dried Ginger—to specifically counteract the Qi stagnation and Blood Deficiency often seen as PMS worsens with age. It is the best tea for pms mood swings because it addresses the root causes of hormonal imbalance, stress, and poor circulation simultaneously.
FAQ
Q: At what age does PMS peak?
A: There is no fixed age range for this, but most women tend to experience it between the ages of 30 and 40. This is because as one gets older, the hormones in the body become increasingly unstable, which is the main cause of PMS symptoms. The premenstrual syndrome (PMS) in women around 20 years old is usually not very pronounced. If it does occur, it is advisable to seek medical attention immediately.
Q: Is there a connection between menopause and PMS? What are the differences between them?
A: Menopause (especially the perimenopausal period) tends to exacerbate PMS symptoms because the unstable changes in hormone levels simulate and intensify premenstrual symptoms. However, menopausal symptoms, such as hot flashes, are persistent, unpredictable, and mark the end of the cycle, whereas PMS is different in that it is cyclical and related to the menstrual cycle, and it has periodic and menstruation-related characteristics, while menopause ends the premenstrual syndrome but brings about more persistent changes. PMS is related to the monthly hormonal changes before menstruation; perimenopause involves a broader and irregular hormonal chaos throughout the entire month, leading to symptoms such as hot flashes, night sweats, dizziness, and vaginal dryness, which are not typical of PMS.
References
- Sood, R., et al. (2018). Premenstrual Syndrome and Premenstrual Dysphoric Disorder: A Systematic Review. *Mayo Clinic Proceedings*, 93(7), 932-945.
- Freeman, E. W., et al. (2019). Symptoms of anxiety and depression in the ovarian hormone withdrawal phase of the menstrual cycle in perimenopausal women. *The Journal of Clinical Endocrinology & Metabolism*, 104(9), 3986-3995.
- Huo, L., et al. (2007). Treatment of premenstrual dysphoric disorder with continuous compared with standard oral contraceptives: a randomized controlled trial. *American Journal of Obstetrics and Gynecology*, 196(4), 304.e1-304.e7.
- Crosby, H., & Rothman, M. (2020). The Impact of Chronic Stress on Hormonal Balance: Implications for Reproductive Health. *Current Opinion in Endocrinology, Diabetes and Obesity*, 27(6), 406-412.
- Yonkers, K. A., et al. (2008). The clinical practice of recognizing and treating premenstrual dysphoric disorder. *Journal of Clinical Psychiatry*, 69(8), 1181-1191.
- Parazzini, F., et al. (2017). Lifestyle and diet and premenstrual syndrome. *Gynecological Endocrinology*, 33(8), 585-589.
- Ozgoli, G., et al. (2009). The effect of ginger for the treatment of primary dysmenorrhea. *Journal of Alternative and Complementary Medicine*, 15(2), 129-132.
- Ahangari, R., et al. (2019). The effects of aromatherapy massage with rose essential oil on the severity of pain and anxiety in women with primary dysmenorrhea. *Complementary Therapies in Clinical Practice*, 34, 21-25.
- Steiner, M. (2000). The neurobiology of premenstrual dysphoric disorder: focus on the role of serotonin, gamma-aminobutyric acid, and the HPA axis. *Journal of Clinical Psychiatry*, 61(Suppl 12), 19-26.
- Ferreira, F. A., et al. (2021). The effects of combined herbal medicine therapy for premenstrual syndrome: A systematic review and meta-analysis of randomized controlled trials. *Phytomedicine*, 80, 153396.
- Kaur, P., et al. (2022). Endometriosis and hormonal interactions in aging women: a clinical perspective. *Climacteric*, 25(1), 101-107.
⚠️ Important Medical Disclaimer
The information provided is for educational purposes only. Do not self-diagnose severe symptoms. If you are experiencing intense pain, severe mood changes, or symptoms that drastically impact your daily life, please consult with a qualified healthcare professional.
About the Author
Laicuherb
The core content team at Laicuherb is a collective of experts, including health professionals, consultants in Traditional Chinese Medicine, and experienced content strategists. Some articles are authored by our brand's founders or R&D scientists. OLaicuherbur team has deep expertise in herbal health, integrating the wisdom of traditional medicine, modern nutrition, and women's health research to transform ancient wellness principles into practical, accessible content for everyday life.








